17 August 2022 at 11:15:50
treat sepsis, obtain baseline bloods, VBG, limb x ray
Refer to Ortho oncall
Necrotising fasciitis is a life-threatening subcutaneous soft-tissue infection that may extend to the deep fascia, but not into the underlying muscle. It is a life and limb-threatening condition with high mortality rates. There are 2 main types based on causative microorganisms
type 1 = polymicrobial (aerobic and anaerobic)
type 2 = monomicrobial (mostly Beta-haemolytic Group A strep)
Clinical suspicion and early recognition are crucial to management
Diagnosis is made clinically. Suspicious features include:
rapid spreading cellulitis with signs of sepsis
disproportionate pain on palpation (due to fascial plain spread)
severe cellulitis with tissue blistering, crepitus, necrosis
radiological appearance of gas in soft tissue (not always present)
Risk factors: diabetes, liver cirrhosis, chronic heart failure, obesity, alcohol abuse, immunodeficiency, systemic lupus erythematosus, Addison’s disease, pre-existing hypertension, and peripheral vascular disease

The LRINEC score (Laboratory Risk Indicator for Necrotising Fasciitis) can be helpful for diagnosis. (but not for ruling out necrotising fasciitis) You will need the CRP, WCC, Hb, Sodium, Creatinine, and Glucose levels for this calculation.
A&E management
refer to Ortho oncall for urgent assessment
ensure the following are undertaken:
mark out the area of cellulitis (indicating the time of marking for later comparison)
Bloods (CRP, WCC, Hb, Sodium, Creatinine, and Glucose levels)
XR of limb
resuscitation and treatment of Sepsis (involve outreach / ITU if indicated)
commence IV antibiotics as per MTW guidelines
Ortho management
assess the patient urgently
if a clinical diagnosis of necrotising fasciitis is made, then arrange for urgent surgical debridement
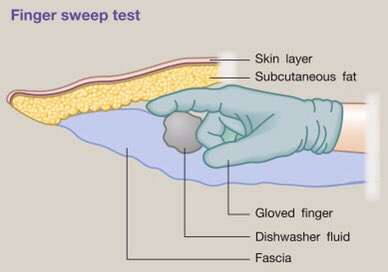
if the clinical assessment is inconclusive, then consider the finger sweep test